Introduction
Clinicians in the emergency department and other acute care settings frequently encounter patients who have sustained trauma to the lower leg or foot and require anesthesia for repair.
Regional block of the saphenous nerve, a pure sensory nerve of the leg, allows for rapid anesthetization of the anteromedial lower extremity, including the medial malleolus. Regional blocks have several advantages compared with local infiltration, such as fewer injections required to attain adequate anesthesia, smaller volume of anesthetic required, and less distortion of the wound site. Because of the lower number of injections, this procedure is better tolerated by the patient and limits the chance of a needlestick injury to the provider.
The saphenous nerve block is gaining popularity not only for procedural anesthesia but also for treatment of pain after procedures. Recently, its use has been demonstrated to be an effective regional technique for post-meniscectomy pain.
While the saphenous nerve can be blocked above the knee, at the level of the knee, below the knee, or just above the medial malleolus, this nerve is commonly blocked at the ankle because of its predictable and superficial location.
Anatomy
Understanding the anatomical distribution of the saphenous nerve helps when performing a successful saphenous nerve block. The saphenous nerve is a cutaneous branch of the femoral nerve originating from the L2-L4 nerve roots. It descends anteroinferiorly through the femoral triangle, lateral to the femoral sheath, accompanying the femoral artery in the adductor canal, and then courses between the sartorius and gracilis muscles across the anterior thigh.

Descent of the saphenous nerve down the anteromedial aspect of the leg.
After piercing the deep fascia on the medial aspect of the knee, the nerve courses superficially down the anteromedial lower leg. The infrapatellar branches supply innervation to the knee. The saphenous nerve runs laterally alongside the saphenous vein, giving off a medial cutaneous nerve that supplies the skin of the anterior thigh and anteromedial leg. The saphenous nerve travels to the dorsum of the foot, medial malleolus, and the area of the head of the first metatarsal. At the level of ankle, the saphenous nerve is found between the medial malleolus and the anterior tibial tendon, just lateral to the saphenous vein.

Saphenous nerve dermatome of the anteromedial leg.

Saphenous nerve dermatome at the level of the foot.
Indications
- Wound repair or exploration of the medial malleolus or anteromedial lower extremity
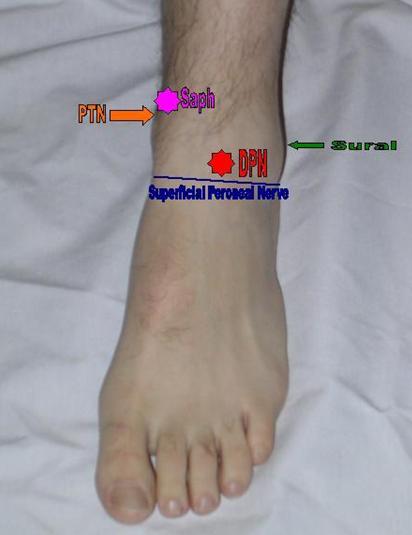
- As part of an ankle block required to manipulate a fractured or dislocated ankle (A combination of posterior tibial, saphenous, superficial peroneal, deep peroneal, and sural nerve blocks results in complete block of sensory perception beneath the ankle.)

Areas of anesthetization to complete an ankle block. This block requires anesthetization of 5 nerves for complete sensory block below the ankle. The areas to anesthetize include a line along the anterior ankle for the superficial peroneal nerve (blue line), the deep peroneal nerve (red star), the saphenous nerve (pink star), the sural nerve (green arrow), and the posterior tibial nerve (orange arrow).
- Incision and drainage of an abscess in the medial malleolus or anteromedial lower extremity
- Foreign body removal in the anteromedial lower extremity or medial malleolus
- Pain after partial meniscectomy
Contraindications
- Allergy to anesthetic solution or additives (eg, ester, amide)
- Overlying cellulitis
- Severe bleeding disorder or coagulopathy
- Preexisting neurological damage
- Patient uncooperativeness (Pediatric or elderly patients may need sedation.
Anesthesia
- Lidocaine, the most commonly used anesthetic, has a fast onset of action and a duration of action of 30-120 minutes, which is increased to 60-400 minutes with the addition of epinephrine. The total cumulative dose of lidocaine to be infiltrated is 4.5-5 mg/kg (not to exceed 300 mg) if lidocaine without epinephrine is used, and 7 mg/kg (not to exceed 500 mg) if lidocaine with epinephrine is used.
- Newer studies have shown that the addition of clonidine 100 mcg to 30 mL of 0.375% bupivacaine (with 5 mcg/mL epinephrine) significantly prolongs duration of the block. The use of clonidine is not yet well-studied, and the authors cannot recommend its use as standard of care at this time.
- Topical anesthetics may be needed in children or uncooperative adults.
Equipment
- Needle, 4 cm, 25 gauge (ga)
- Needle, 18 ga
- Syringe, 10 mL
- Marking pen
- Sterile gloves
- Antiseptic solution (povidone [Betadine] or chlorhexidine gluconate [Hibiclens]) with skin swabs
- Alcohol swabs
- Sterile drape
- Lidocaine 1%, 10 mL
- Facial mask with eye shield
- Sterile gauze
Positioning
- Position the patient supine with the leg externally rotated and the ankle elevated (if anesthetizing at the level of the ankle) or knee elevated (if anesthetizing at the level of the knee).
- Alternatively, the patient may sit and face the clinician.
Technique
Explain the procedure, benefits, risks, and complications to the patient and/or patient’s representative, and inform the patient of the possibility of paresthesia during the procedure.
Obtain informed consent in accordance with hospital protocol.
Perform and document neurovascular and musculoskeletal examinations prior to the procedure. Testing the saphenous nerve prior to block includes sensation of anteromedial thigh and lower leg.
Knee level
Expose the knee and palpate to identify the medial femoral condyle and the medial tibial condyle.

Identify the landmarks: medial femoral and tibial condyles.
Prepare the site with antiseptic solution. While maintaining sterile technique, place a skin wheal of local anesthetic using a 25-ga needle.

Antiseptic (Betadine) preparation.
Subcutaneously infiltrate 7-10 mL of local anesthetic solution in a transverse line from the posteromedial to the anteromedial aspect of either condyle.

Anesthetize posteromedial to anteromedial at either condyle.
If the leg does not need to be anesthetized, use the saphenous block technique for the level of the ankle.
Ankle level
Expose the area of injection and identify the landmarks. Start by palpating the medial malleolus and the great saphenous vein at the ankle. Mark the site 1.5 cm superior and anterior to the anterosuperior border of the medial malleolus.

Mark the site 1.5 cm superior and anterior to the medial malleolus.
Advance laterally in a transverse line toward the lateral malleolus to identify the anterior tibial tendon while the foot is in dorsiflexion (dorsiflexion exaggerates the tendon). Also identify the anterior tibial ridge by advancing further in the transverse line while the foot is in plantar flexion. A divot in the anterior ankle can be felt before the contribution by the fibula is met.

The divot between the anterior tibial tendon and the tibial ridge.
Prepare the site with antiseptic solution. While maintaining sterile technique, place a skin wheal of local anesthetic using a 25-ga needle.
Advance the needle through the skin wheal toward the anterior tibial tendon in a superficial transverse line, without injecting the tendon itself.

Saphenous nerve anesthetization site.
In some instances, further anesthesia is necessary (to the anterior tibial ridge) to get a complete block of the area.
Calor and rubor of the foot due to loss of sympathetic tone may initially be noted.
Pearls
- Equipment preparation and proper patient positioning may make the difference between success and failure.
- In children or noncompliant adults, consider using topical anesthetic mixtures, such as lidocaine, epinephrine, tetracaine (LET) or a eutectic mixture of lidocaine and prilocaine (EMLA cream).
- Pediatric or elderly patients may require additional sedation for compliance.
- Consider a hematoma block or bier block when a fracture exists or when more extensive manipulation of the foot is expected.
- Adding a buffering solution, like sodium bicarbonate, can significantly decrease the pain of the injection when performing a nerve block. Add 1 mL of sodium bicarbonate (44 mEq/50 mL) to 9 mL of lidocaine.
- Warming the anesthetic solution to body temperature can significantly decrease the pain of the injection.
- When unassisted, tape a bottle of lidocaine upside down to the wall prior to the procedure. If more anesthetic is needed during the procedure, it can be obtained from this bottle without compromising the sterility of gloves and equipment.
Complications
- Infection: Infection occurs when the puncture site is not clean. Avoid puncture through infected skin or skin lesions. Be sure to use sterile technique during the procedure, as the risk of infection is insignificant when sterility is properly maintained.
- Intravascular injection: Intra-arterial injection may result in vasospasm and lead to ischemia of the limb tissue. Intravenous injection can lead to systemic toxicity when high doses of anesthesia are injected. Tissue texture changes revealing pallor, bogginess, and cool temperature may indicate that either intravascular injection or vascular compression has occurred. Always aspirate the syringe to rule out intravascular placement before injection. Alpha-adrenergic antagonists (eg, phentolamine 0.5-5 mg diluted 1:1 with saline) can be administered by local infiltration to relieve arterial vasospasm secondary to intra-arterial injection.
- Nerve injury: Patients may develop paresthesia, sensory deficits, or motor deficits secondary to inflammation of the nerve. Most often, this type of neuritis is transient and resolves completely. During the procedure, pull back gently after induction of paresthesia so as to not inject the nerve directly. Make sure to document a complete neuromuscular examination both before and after the procedure.
- Hemorrhage: Reports of significant hemorrhage during regional anesthesia are rare, even in patients with blood coagulopathies. A hematoma may develop with intravascular puncture. If prolonged bleeding occurs, attempt to obtain hemostasis with direct pressure and elevation.
- Allergic reaction: Allergic reactions to local anesthetics occur at a rate of 1%. Reactions range from delayed hypersensitivity (Type IV) to anaphylactic (Type I). Although rare, the most common cause of allergic reaction to anesthetics is the preservative in the local anesthetic solution. Using cardiac lidocaine is an alternative, as it does not contain the preservative (eg, methylparaben). Alternatively, a 1-2% diphenhydramine solution can be used as a local anesthetic.
- Exceeding total volume of anesthesia: The volume of 1% lidocaine without epinephrine should not exceed 5 mg/kg. If lidocaine with epinephrine is used, total volume should not exceed 7 mg/kg. Systemic toxicity manifests in the central nervous and cardiovascular systems. Signs such as tremors, convulsions, tachycardia, or respiratory compromise should alert the clinician to stop the procedure and reassess the patient.
Ultrasonographic Guidance
The use of ultrasound-guided techniques for regional anesthesia is becoming more popular. Ultrasonographic guidance is best for blocking the saphenous nerve when palpation of the saphenous vein is difficult. Despite tourniquet use or leg dependency, palpating the vein as a landmark may not be possible (eg, common in patients who are obese). In these situations, the use of ultrasonographic guidance is prudent. An additional advantage of this approach is to avoid puncturing the saphenous vein, especially at the level of the knee.
Paravenous approach at the level of the knee
- This technique is well-described by Andrew Gray and Adam Collins.
- A short-axis view of the saphenous vein is employed, with the needle directed nearly parallel to the transducer within the plane of imaging.
- The approach begins at the level of the tibial tuberosity, with the needle entry site anterior to the aspect of the medial leg.
- Using a high frequency linear probe, identify the saphenous vein and the fascia lata.
- The goal is local anesthetic infiltration between these two landmarks on ultrasound.
- A 25-gauge needle can then be directed in a posterolateral fashion to approach the nerve.
Adductor canal approach at the level of the knee
- This approach is well-described by Jens Krombach and Andrew Gray.
- Use a 14-MHz linear ultrasound transducer and scan the medial thigh 5-7 cm proximal to popliteal crease.
- Slide the probe until the image of the adductor canal is obtained.
- The saphenous nerve can be imaged where it pierces the membrane.
- Recall that the saphenous nerve travels deep to the sartorius muscle adjacent to the descending branch of the femoral artery, which may be seen with power Doppler.
- The saphenous nerve emerges between the sartorius and gracilis muscle tendons, piercing the fascia lata to join the saphenous vein within subcutaneous tissue.
- Infiltrate 5-10 mL of local anesthetic adjacent to the saphenous nerve deep to the sartorius muscle.
Approach at the level of the ankle
Ultrasonographic guidance may also be employed at the ankle to identify the saphenous vein when it cannot be identified by visualization or palpation. This can serve as a starting point for identifying the landmarks (see Technique above). However, the saphenous nerve is usually not visible with ultrasound imaging at this level; therefore, the procedure typically relies on the landmarks.
A disadvantage of the ankle block is that it usually requires large volumes of local anesthetic. According to Frederickson, these volumes can be reduced with the use of ultrasonographic guidance because of the more precise needle placement and real-time repositioning that such guidance allows. This reference paper states that typical volumes of 30 mL can be reduced to 15 mL for the entire ankle block.
Four of the five nerves in the ankle block can be approached with an in-plane needle transducer orientation directly, using a vessel as a guide, except for the superficial peroneal nerve. These nerves and their corresponding vessels are as follows:
- Deep peroneal nerve – Lateral to anterior tibial artery
- Posterior tibial nerve – Posterior to posterior tibial artery
- Saphenous nerve – Adjacent to the long saphenous vein
- Sural nerve – Adjacent to the short saphenous vein
The saphenous nerve can be approached with a narrow curvilinear probe to allow a direct tangential needle approach. Please refer to Frederickson's paper, which diagrams this nicely.
Source Emedicine.medscape.com
Originally posted 2010-09-22 12:56:17.